Background/Aims: The aim of the present study was to demonstrate the histopathological findings in gastrointestinal (GI) biopsies in adults with common variable immunodeficiency (CVID).
Materials and Methods: A total of 172 GI biopsies of 26 patients with CVID obtained over a 16-year period were reevaluated. Findings were analyzed using descriptive analyzes and χ2 test.
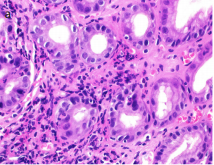
Results: Female-to-male ratio was 1.36. The median age at diagnosis was 36±13.94 (16-72) years. Chronic esophagitis was noted in 3 patients. The absence of plasma cells in the stomach, duodenum, and colon was observed in 16, 14, and 9 patients, respectively. Divergent results for the presence of plasma cells in concurrent stomach and duodenum samples were found in 11 (44%) patients. Nodular lymphoid hyperplasia (NLH) was notable in the duodenum (56%). The mean number of eosinophils in one high-power field was significantly higher in duodenal biopsies with NLH (27.21 vs. 14.37, p=0.002). Active inflammation was more prominent in the colon (91%) than in the stomach (65%) and duodenum (60%). Helicobacter pylori infection was found in 57.6%, including a case with persistent infection by the coccoid form. Celiac-like villous blunting and increased intraepithelial lymphocytes were seen in 40% and 24%, respectively. In addition, 23% had giardiasis associated with acute duodenitis and duodenal NLH (p<0.05).
Conclusion: CVID gastroenteropathy is a challenging entity, and due to the heterogeneity in the presence and distribution of plasma cells throughout the GI tract and diverse disease course, multiple concurrent biopsies may be needed for tissue diagnosis. Duodenal CVID may present with villous alterations and giardiasis, and NLH appears to be an important clue in the duodenum. The association between duodenal NLH and eosinophil infiltration deserves further investigation.
Cite this article as: Pehlivanoğlu B, Ardeniz Ö, Hassoy H, et al. Gastrointestinal findings in 26 adults with common variable immunodeficiency: The fickle nature of the disease manifests in gastrointestinal biopsies. Turk J Gastroenterol 2019; 30(9): 789-800.




.png)
.png)